Principles of Flexibility
To fully understand the concepts of flexibility training and how a muscle lengthens, it is necessary to have a thorough understanding of muscle architecture. This section will provide a basic overview of the physiology of flexibility.
Anatomically, muscles share common characteristics at the cellular level, although they come in many sizes and perform various functions.
Muscle Tissue
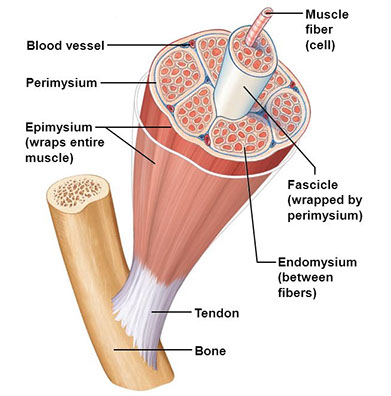
Muscle tissue is composed of strands of tissue called fascicles. The individual fascicle is comprised of fasciculae, which are bundles of muscle fibers. Muscle fibers are composed of thousands of myofibrils, which contain the contractile components of the muscle tissue.
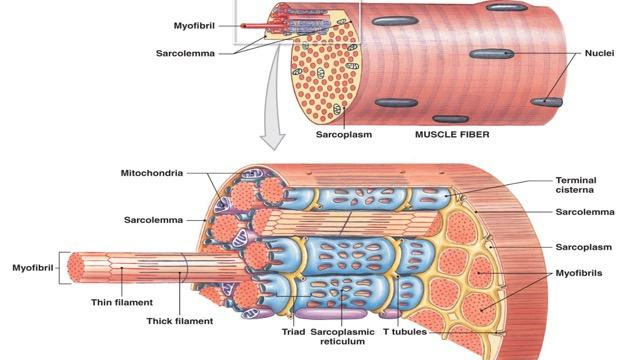
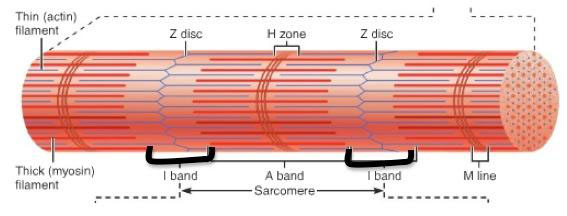
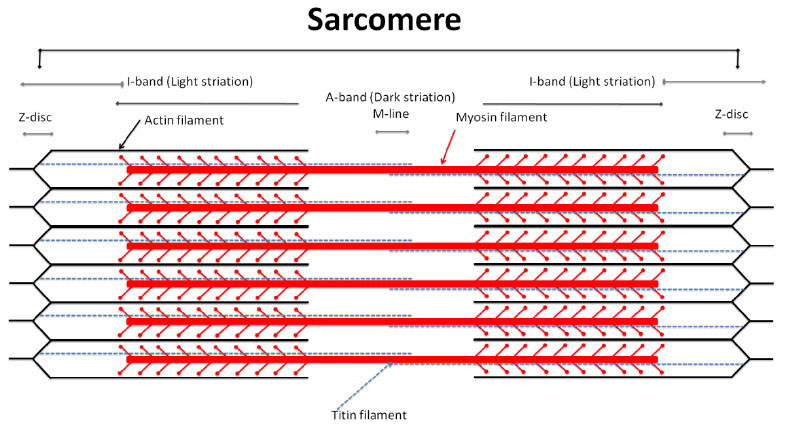
The myofibrils are composed of microscopic bands called sarcomeres. Each sarcomere is made up of myofilaments, which include overlapping thick and thin contractile proteins, primarily actin and myosin.
The process of muscular contraction occurs when a neural impulse (action potential) from the brain crosses the neurosynaptic junction. This impulse stimulates the cellular exchange of calcium and potassium, which causes the thick and thin myofilaments to slide by one another, causing the sarcomere to shorten.
Muscle fibers always contract completely. This is known as the All-Or-None Principle. Each fiber is unable to vary the intensity by which it contracts. If the action potential is strong enough to induce contraction, it will contract completely. The greater the number of muscle fibers that are recruited, the greater the force produced.
Sliding filament theory is the proposed process of how the contraction of the filaments within the sarcomere takes place.
Steps in the sliding filament theory are summarized as follows:
A sarcomere shortens as a result of the Z lines moving closer together.
The Z lines converge as the result of myosin heads attaching to the actin filament and asynchronously pulling (power strokes) the actin filament across the myosin.
The I band and H zone will converge as they are comprised of the moving actin filament and the A band will remain the same as it is comprised of the stationary myosin filament.
Connective Tissue
Connective tissue encases the muscle tissue and its fibers. Connective tissue is composed of two types of protein-based fibers.
1. Collagenous Connective Tissue
2. Elastic Connective Tissue
Collagenous Connective tissue is composed mainly of a strong, inelastic compound called collagen. Elastic Connective tissue contains elastin, which is an extensible protein, and is capable of stretching. Connective tissues include:
1. Tendons
2. Ligaments
3. Fascia
Fascia binds muscles into separate groups. There are three layers to the fascial sheaths, named according to the structures they surround:
1. Endomysium
2. Perimysium
3. Epimysium
Endomysium is the innermost fascial layer that encases individual muscle fibers. The sheath that binds groups of muscle fibers into fasciculi is called Perimysium. The outermost layer of fascia is the Epimysium. This layer binds entire fascicles together. These connective tissues must also respond to flexibility training for permanent changes (Plastic Deformation) to occur. Overuse injuries initiate the Cumulative Injury Cycle, which stimulates the development of inelastic, fibrous adhesions. These adhesions form in the connective tissue between layers of muscle. This prevents normal muscle mechanics and normal soft tissue extensibility.
All tissues contribute to joint stiffness to different degrees:
47% Joint capsule and ligaments
41% Fascia
10% Tendons
2% Skin
(Ref. Johns RJ, Wright V. The Relative Importance of Various Tissues in Joint Stiffness, 1962)
Although the myofascial system ranks second, it should be the focus of a flexibility program. Tissue properties of the muscle and fascia allow for greater elasticity, and a greater adaptive potential than ligamentous tissue. Furthermore, tendons are biologically designed to contain less elastic tissue than muscle.
Over-stretching ligaments can produce unstable joints. This can alter the normal length-tension relationships, farce-couple relationships, and joint arthrokinematics, which leads to synergistic dominance and faulty movement patterns. This initiates the Cumulative Injury Cycle and places unwanted stress on the entire kinetic chain. You must keep in mind the myofascial, neural, and vascular structures that incur stress as a result of an applied stretch, then design a flexibility routine accordingly.
Neurodynamics
All neural tissue has to adapt to constantly changing joint angles and alterations in the position of the adjacent tissue. Muscle imbalances, joint dysfunctions, and postural distortions place abnormal tension on the neural tissues. This inturn affects the structural integrity of the neural structures and leads to abnormal neurodynamics.
The Peripheral Nervous System
The peripheral nervous system (PNS) includes:
1. The Spinal Cord
2. Spinal Nerve Roots
3. Spinal Meninges
4. Root Ganglion
5. Spinal Nerve
The peripheral nerve trunk is composed of the nerve fibres, blood vessels, and connective tissues. The connective tissues that surround the nerve fibres include:
1. Perinerium
2. Epinerium
3. Endonerium
4. Mesonerium
These connective tissue structures form a tough, supporting framework for the contained neurovascular triad. The neural connective tissues are self innervated by the nervi nervorum. This innervation, along with an abundant blood supply, makes the connective tissue of the nerve very reactive and pain sensitive.
Neuropathophysiology
Acute injury (compression), chronic injury (repetitive microtrauma), muscle imbalances, joint dysfunctions, and poor posture compromise the integrity of the neural tissues. Any tissue trauma initiates a neurogenic reflex mechanism, the cumulative injury cycle and creates morphological changes in the microenvironment of the neural tissue. This results in intraneural edema, chemical irritation, tissue hypoxia, and microvascular stasis.
All of these alterations stimulate the nocioceptors and result in pain. Pain causes protective muscle spasms to decrease the provocation to the inflamed neural tissues, which causes altered length-tension relationships, force couple relationships, joint arthrokinematics, and altered movement patterns. This process eventually leads to intraneural fibrosis, which decreases neural tissue elasticity.
This prevents normal neurodynamics during functional movements and further perpetuates the dysfunctional cycle.
You should be able to assess the neural tissue for abnormal provocation prior to initiating an aggressive fitness and conditioning program. It is important to differentiate between flexibility deficits and abnormal neural tension. It is very important to determine if the neural tissue has optimum elasticity during multi-planar functional movements.
During the Functional Integrated Assessment the individual should perform passive or active movements. These movements impart tension to the pathological neural tissue. The tension is provocative, causing pain, muscle tone changes, limited range of motion, and neural symptoms (numbness and tingling).
Muscle stretching or elongation essentially begins with the sarcomere, the contractile component of muscle tissue. As the sarcomere contracts, thick and thin myofilaments slide closer together and overlap. Upon stretching, the overlap in the sarcomere decreases, which allows the muscle fibre to elongate. Once the sarcomeres are fully stretched out, additional elongation comes from the surrounding connective tissue (fascia and muscle tendons).
Davis’ Law states that soft tissue models along the lines of stress; this is an important concept when considering the nature of soft tissue following injury.
An increase in scar tissue is present following an injury secondary to the cumulative injury cycle. Scar tissue has many inelastic properties, but will realign its fibers into functional lines of stress with proper flexibility training.
Flexibility Training not only affects the muscular system, but also affects the neural system through two basic forms of feedback:
1. Recruitment
2. Rate Coding
3. Recruitment
An impulse transmitted simultaneously over a varying number of nerve fibers. This is sensitive to the stretch intensity and the number of fibers recruited.
For example, a moderate straight-leg raise hamstring stretch will only stimulate a few stretch receptors. But as the stretch intensity increases, a greater number of receptors are stimulated.
Rate Coding
A time-sensitive feedback mechanism. This is when the same nerve fiber transmits impulses per unit of time. As the stretch intensity increases, so does the frequency of the impulse being sent to the spinal cord, which will usually result in some form of motor response (stretch reflex).
Sensors within the musculotendinous unit provide the neural feedback. These sensors are collectively called mechanoreceptors. There are three basic types of mechanoreceptors:
1. Muscle spindles
2. Golgi tendon organs
3. Joint mechanoreceptors.
4. Muscle Spindles
The major sensory organs of the muscle and are composed of microscopic intrafusal fibers that lie parallel to the extrafusal muscle fibers. Muscle spindles are sensitive to change in length and rate of length change.
When a muscle is stretched, the intrafusal and extrafusal fibers of that muscle are stretched concurrently.
Golgi Tendon Organs (GTO)
The Golgi tendon organs are located within the musculotendinous junction and sensitive to changes in tension and rate of tension change. Prolonged GTO stimulation provides inhibitory action to muscle spindles (located within the agonist muscle).
This neuromuscular phenomenon is called autogenic inhibition. This process occurs when the neural impulses sensing tension are greater than the impulses causing muscle contraction. The phenomenon is termed autogenic because the contracting agonist is inhibited by its own receptors. The other receptors include joint mechanoreceptors.
As the name implies, these are located in joints throughout the fibrous capsule and ligaments. These receptors signal joint position, movement and pressure changes.
The Stretch Reflex
A reflex is a neuron circuit consisting of a sensory neuron, communicating neuron and a motor neuron with its effector muscle. When a stimulus is applied to the receptor ending an impulse is created. This impulse travels to the spinal cord where a motor neuron is excited.
The nerve impulse is conducted to the effector site on the muscle and a motor response is initiated. A reflex is a response to the stimulus. As the stimulus intensity increases, the motor response (reflex) is proportional. When extrafusal muscle fibers are stretched, the intrafusal (muscle spindles) fibers are also stretched. These relay information regarding changes in muscle length and rate of change of muscle length. They produce a motor response, also called a myotatic stretch reflex.
When a muscle is stretched very quickly, the muscle spindle contracts, which in turn stimulates the primary afferent fibers that causes the extrafusal fibers to fire and tension increases in the muscle (myotatic stretch reflex).
The rationale for holding a stretched position is to stimulate the GTO’s inhibitory action to the muscle spindles, which will allow adaptive changes to muscle spindle sensitivity at the new range. If a slow stretch force is applied to muscle, the GTO fires and inhibits the tension in the muscle, allowing the parallel (sarcomere) and series elastic elements to elongate.
This myotatic stretch reflex has a static (tonic) and dynamic (phasic) component. The tonic portion remains as long as the stretch is active. The phasic component is proportional to the velocity of the stretch. These neurophysiological principles must be understood so they may be properly administered in a successful flexibility program.
Factors Limiting Flexibility
Factors that limit flexibility vary on an individual basis and may be affected by internal and external influences. These factors need to be taken into consideration when designing a flexibility program.
Internal Influences Limiting Flexibility:
– Type of joint (some joins are genetically limited for stability, the sacroiliac joint for example).
– Certain bony structures limit movement (Ulnar olecranon for example).
– Elastic nature of soft tissue (previously injured tissue is high in scar tissue which is very inelastic).
– The joint’s internal resistance (fibrous capsule).
– Elasticity of skin (skin is very rich with mechanoreceptors which provide continual biofeedback).
– Elastic nature of ligaments and tendons (ligamentous laxity is a precursor to joint hypermobility which may cause injury).
– Neuromuscular efficiency.
– Weakness in the antagonist musculature.
– Hydration (and Nutrition).
– Temperature of soft tissue and joint (body is more flexible following proper warm-up exercises).
– Pre-existing injuries, muscle imbalances, tender points.
– Postural malalignment. Congenital or acquired.
External Influences Limiting Flexibility:
– Temperature of training venue (usually warmer climates are more appropriate for increasing flexibility).
– Age (flexibility naturally declines during the aging process).
– Technical skill level (poor motor patterns do not produce optimal levels of functional flexibility).
– Time of day (most people are most active in the afternoon).
– Psychological restraints (one’s commitment to increasing flexibility).
– Equipment or clothing restrictions.
Some sources also suggest that water is an important dietary element with regard to flexibility. Increased water intake is believed to contribute to increased mobility, as well as increased total body relaxation.
Indications for the use of stretching procedures:
– When ROM is limited because soft tissues have lost their extensibility as the result of adhesions, contractures, and scar tissue formation, causing functional limitations or disabilities.
– When restricted motion may lead to structural deformities otherwise preventable
– When there is muscle weakness and shortening of opposing tissue
– As part of total fitness program designed to prevent musculoskeletal injuries
– Prior to and after exercise to potentially minimize post exercise muscle soreness and aid in recovery
– Prior to and potentially after exercise to decrease risk of injury
(Ref: Indications for use of stretching (Kisner C, Colby L: Therapeutic Exercise. Foundations and Techniques; (4th Edition); 2002)
Contraindications for the use of stretching procedures:
– When a bony block limits joint motion
– After a recent fracture before bony union is complete
– Whenever there is evidence of an acute inflammatory or infectious process (heat and swelling) or when soft tissue healing could be disrupted in the tight tissues and surrounding region
– Whenever there is sharp, acute pain with joint movement or muscle elongation
– When a hematoma or other indication of tissue trauma is observed
– When hypermobility already exists
– When contractures or shortened soft tissues are providing increased joint stability in lieu of normal structural stability or neuromuscular control
– When contractures or shortened soft tissues are the basis for increased functional abilities, particularly in clients with paralysis or severe muscle weakness
